|
|
POLYSOMNOGRAPHY - SLEEP APNOEA:
 Sleep
apnoea (apnea - US spelling) is a breathing disorder that
occurs in sleep. There are two main types of sleep apnoea;
obstructive sleep apnoea and central sleep apnoea, though it
is possible to have a combination of both causes. Narcolepsy
is another sleep disorder but sleep apnoea must be ruled out
before it can be diagnosed along with other more specialised
tests (see Neurophysiology). Sleep
apnoea (apnea - US spelling) is a breathing disorder that
occurs in sleep. There are two main types of sleep apnoea;
obstructive sleep apnoea and central sleep apnoea, though it
is possible to have a combination of both causes. Narcolepsy
is another sleep disorder but sleep apnoea must be ruled out
before it can be diagnosed along with other more specialised
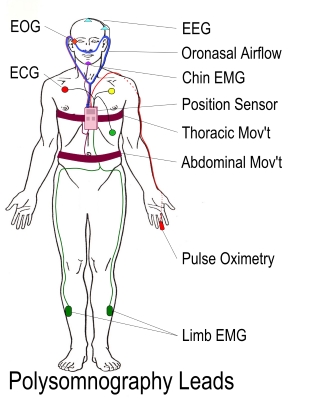
tests (see Neurophysiology).The most commonest sleep apnoea is obstructive sleep apnoea (OSA). This is where there is a partial obstruction (hypopnoea) or complete obstruction (apnoea) causing a significant reduction in the airflow or complete occlusion in the presence of normal breathing effort. The most likely cause for this is upper airway collapse. During these apnoeas Oxygen desaturation is seen and can lead to arousal from sleep. Central sleep apnoea is much less common than OSA and this is where the autonomic system stops sending signals to the muscles that control breathing, as the breathing is stopped oxygen desaturation can also occur. This type of apnoea occurs when there is damage to the brainstem from infection, haemorrhage or trauma to the cervical spine (neck). Other causes can include Parkinson's disease, cardiac failure and side effects of some medications such as narcotic painkillers. As previously mentioned there can be a combination of OSA and central sleep apnoea and this is most likely caused by obesity amongst other causes Testing for sleep apnoea falls into two general categories: polysomnography and limited channel monitoring (also known generically as 'sleep apnoea testing'). Sleep Questionnaires and Diaries also provide useful information to understand a person's sleep habits and patterns. The commonest in use in UK is the Epworth Sleepiness Scale. However, by themselves they are insufficient to confirm or exclude the diagnosis of OSA. Epworth Sleep Scale Polysomnography
Polysomnography simultaneously records multiple physiological signals during sleep. The parameters that are recorded during polysomnography may include all or most of the following:
Limited Channel Monitoring or Sleep Apnoea Test
Increasingly, people who have a high likelihood of OSA and have few other medical conditions after a clinical consultation, are tested via limited channel monitoring. This method is also used as a means to determine whether their treatments are effective.
Results
Apnea Hypopnea Index (AHI). The AHI is the number of apnoeas or hypopnoeas that are recorded during the study per hour of sleep. It is generally expressed as the number of events per hour. Respiratory Disturbance Index (RDI. This is slightly different to the AHI as the RDI includes not only apnoeas and hypopnoeas, but it also includes respiratory effort related arousals (RERA's). RERAs are arousals from sleep that do not technically meet the definitions ofapnoeas/hypopnoeas but do disrupt sleep. They are abrupt transitions from a deeper stage of sleep to a shallower one. This means a person's RDI can be higher than their AHI. Both the AHI and RDI sleep apnoea severity is classified as follows: None/Minimal: AHI < 5 per hour Mild: AHI ≥ 5, but < 15 per hour Moderate: AHI ≥ 15, but < 30 per hour Severe: AHI ≥ 30 per hour |
Copyright
© 2013 by Lee Boswell
Disclaimer