|
MISCELLANEOUS AUDIOLOGY INVESTIGATIONS:
Speech
Audiometry
The sound of language is how we communicate so therefore the
recognition of speech is considered important. Speech audiometry was
used to cross check pure audiograms in the past and to assist in
conjunction with the pure tone audiogram with the degree and type of
hearing loss. More recently and more commonly Speech Audiometry is used
to assist the correct gain and maximum output levels over various
frequencies for hearing aids.
There are three main investigations concerning Speech Audiometry, these
are:
Speech Detection Threshold (SDT) also called Speech Awareness Threshold
(SAT)
Speech Recognition Threshold (SRT) sometimes called Speech Reception
Threshold
Speech Discrimination Score (SDS) also called Supra-Threshold Speech
Testing.
Speech
Detection Threshold (SDT)
This test uses pre-recorded word lists usually of up to 50 words per
list. Each word is a two equally stressed syllable word that is
familiar to the target population, this is also called a 'spondee'.
Examples of spondee words are: cowboy, hotdog, cupcake, ice cream.
The purpose of the speech detection threshold is to obtain the lowest
level of intensity that someone can detect familiar words at least 50%
of the time. Spondee words are presented, usually two words at each
intensity (though there are other protocols) at a comfortable level, if
the subject hears the word they, respond (by pressing a button). If the
response rate is 50% or better then the intensity of the words
presented is reduced by 10dB. The subject does not repeat the word,
they merely indicate that they have heard it. The SDT should be similar
to the pure tone audiogram threshold.
SDT testing is useful for subjects that may be too young to understand
or repeat the words, for subjects that cannot understand the language
tested (For example Charity organisations working in foreign countries)
or for those that have an impaired language function due to a
neurological injury.
Speech
Recognition Threshold (SRT)
The SRT is used to determine the lowest intensity that someone can
recognise familiar two syllable spondee words 50% of the time. In
addition to determining the softest level at which people can hear and
repeat words the SRT is also used to validate pure tone audiograms.
This is because there is a high correlation between the SRT and the
average of pure tone audiometry at 500, 1000 and 2000Hz. This is called
the Three frequency Average Hearing Threshold (3FAHL).
In practice the SRT is within 5-10dB of the 3FAHL. However if the pure
tone hearing has a sharp loss and one of the frequencies in the pure
tone audiogram is significantly worse than the other two then in this
case the SRT will be better. If the SRT is significantly worse than the
3FAHL then a retrocochlear lesion can be suspected.
SRT is also used to determine the Presentation Level (PL) for Speech
Discrimination Score testing, here, the PL is usually 30-40dB above the
SRT as this has been found to be a comfortable level to start at.
Speech
Discrimination Score (SDS)
 SDS is a good indicator of a person's ability to
communicate at normal conversational levels. It is also able to
indicate whether further diagnostic assessment is required and is
useful in the initial programming of hearing aids for subjects and then
assessing the usefulness of the hearing aid. SDS is a good indicator of a person's ability to
communicate at normal conversational levels. It is also able to
indicate whether further diagnostic assessment is required and is
useful in the initial programming of hearing aids for subjects and then
assessing the usefulness of the hearing aid.
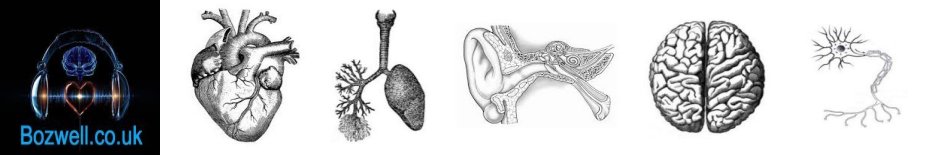
SDS is calculated with the use of single syllable, phonetically
balanced words each with three phonemes or parts to the word, such as
'cat', 'fun', 'shape' and ' guess'. The SRT is calculated and then a
list of 10 words are played to the subject at 30-40dB above the
SRT/3FAHL. The subject has to repeat back the word that they think they
have heard and the tester will write that word down and score each word.
For each Word List there are 10 words, each word is single syllable and
has three phonemes. If the word is repeated back correctly they score
10, if they correctly identify two phonemes they score 7, one phoneme
is worth 3 and if they cannon repeat a word they score 0.
As previously mentioned the intensity level that the initial word list
is presented is at 30-40dB above the SRT, if the Phoneme score is 80%
or better then the intensity is reduced by 10dB and a different word
list is presented at this level and scored again, this process is
repeated until a Phoneme score of 50% is reached.
If the initial Phoneme score was less than 80% then the intensity is
increased by 10dB, a new list used and repeated, until a maximum score
or 100% is obtained. A subject with a sensorineural hearing loss may
not reach 100% so once the maximum Phoneme score has been obtained the
intensity is again increased by 10dB and the word list is scored to see
if the Phoneme score reduces, if the speech discrimination worsens as
the intensity is increased then this is termed 'roll over' and is often
associated with retrocochlear lesions.
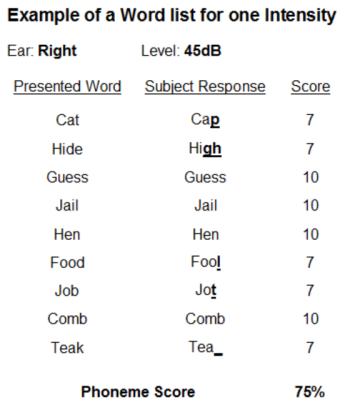
From these results a Speech Curve or Performance Intensity Function
graph can be plotted.
As can be seen from the Speech curve, a normal hearing person
will have 80% or better at around 30dB and most likely 100% at 40dB+. A
conductive loss will still be able to achieve over 80% discrimination
scores but the general loudness will have been increased and as can be
seen on the Speech curve above 80% is achieved at 55dB. A sensorineural
loss may not achieve an 80% discrimination score and if the intensity
is further increased the score can drop, this important when hearing
amplification is considered, merely increasing the amplification will
not increase the discrimination score.
Loudness
Discomfort Level (LDL)
Loudness discomfort level is a subjective measure of a persons
perception to a sound when the stimulus intensity becomes
uncomfortable. In a normal person the LDL is seen at around 80-100dB
above threshold, this threshold to LDL difference is called the dynamic
range.
Recruitment is a persons perception of a disproportionate rapid
increase of loudness for increasing equal steps of intensity, the
result of which would be a reduction in the size of the dynamic range.
This is usually seen in Cochlear losses.
Alternate
Binaural Loudness Balance Test (ABLB)
  This
test is designed to detect recruitment subjectively in unilateral
hearing losses by measuring the difference between both ears in
perceived equal intensity. This test is performed at frequencies with
suspected recruitment, usually higher frequencies. Both ears are
presented with continuous pure tones of the same frequency. The worse
ear (reference) is presented at a stimulus 20dB above the threshold. This
test is designed to detect recruitment subjectively in unilateral
hearing losses by measuring the difference between both ears in
perceived equal intensity. This test is performed at frequencies with
suspected recruitment, usually higher frequencies. Both ears are
presented with continuous pure tones of the same frequency. The worse
ear (reference) is presented at a stimulus 20dB above the threshold.
The task of the subject is to adjust the intensity on the better ear's
side until the presented tones are perceived to be equal in both ears.
The intensity for the better and worse ear is noted then the intensity
of the reference tone is increased by 10dB, this process is repeated
until the stimulus intensity becomes uncomfortable.
Note: The reference tone can also be fixed at 20dB for the good ear and
the subject then matches the intensity on the worse side.
The results are plotted on a graph and any recruitment will easily be
seen as the stimulus intensity increases disproportionately to the good
ear.
Stenger
Test
The Stenger Test is based on the 'Stenger Principle' in that if
continuous pure tones are presented to both ears only the perceived
loudest intensity will be heard by the subject. This means that only
the ear that hears the loudest relative sound will be heard and the
quieter tone, although still present, will not be perceived by the
subject.
This test is useful to confirm unilateral losses but is most useful
when a unilateral non-organic loss or malingering is suspected.
The subject is instructed to press a button whilst they can hear the
tone. A continuous pure tone is presented to the better ear at 20dB
above threshold. The perceived worse ear is presented with a continuous
pure tone at 20db less than the good ear so the subject only hears the
tone in the good ear. The worse ear stimulus is slowly increased and if
the unilateral loss is genuine the subject will continue to hear the
tone in the good ear even when the intensity surpasses that of the good
ear (Negative Stenger). However if the subject is feigning a loss he
will stop responding to the good ear tone when the intensity of the
'worse' ear exceeds that presented to the good ear (Positive Stenger).
Carhart's
Tone Decay
For normal hearing people pure tones that are presented well above
their threshold in the normal audiometric range remain audible and they
experience no (or little) change to the perceived loudness over time.
In some cases of hearing impairment the audible tone decays over time.
Marked tone decay is usually interpreted as a sign of a retrocochlear
dysfunction.
Carhart's Tone Decay test (1957) is performed after normal a normal
audiogram to establish thresholds for both ears. A pure tone is then
presented sub-threshold and increased until the subject hears the tone,
the subject is instructed to continue to press a button whilst they
hear the sound. If they no longer hear the pure tone the stimulus is
increased by 5dB and the timer is reset.
The test terminates when the subject hears the tone for a minute
without having to increase the threshold or the pure tone threshold has
been increased 30dB above the initial subject's response. Multiple
frequencies may be tested for both ears.
If the initial pure tone is heard for 60 seconds or the stimulus is
only increased by 5dB the result is within normal limits. If the
stimulus was increased by 10-15dB this is a mild decay,
20dB or greater is considered a marked decay.
Rosenberg's Tone Decay is a slight variation in that a single
presentation of 1 minute is presented, when the tone becomes inaudible
to the subject the stimulus is increased by 5dB, this is repeated until
1 minute elapses from initial presentation of the pure tone stimulus.
The results are graded by how much/many times the stimulus was
increased in the one minute period.
Short
Increment Sensitivity Index (SISI)
This procedure is designed to assess a subjects ability to determine a
slight increase (1dB) in intensity to a continuous tone that is
presented at 20dB above threshold. A subject with a retrocochlear
disorder will not be able to differentiate the 1dB change in intensity
but a subject with a cochlear lesion will.
The pure tone is presented continuously at 20dB above threshold
(Carrier tone) for a particular frequency (usually 1KHz or 4KHz) and
the subject is instructed to press a button when they can notice a
difference in the loudness. At random times the intensity will be
increased by 1dB for a total of twenty time and subjects response is
recorded and converted to a percentage.
A detection rate of 70% or more is considered a positive result and a
cochlear lesion is suspected, 30% and below the disorder is elsewhere.
Glycerol
test for Ménière's
Although a diagnosis of Ménière's can be made from a subjects history,
examination and audiogram the glycerol test can help to not only
confirm the diagnosis but also to exclude other possible disorders.
Glycerol is ingested at 1.5 g/kg and the audiogram is repeated every 30
minutes for 3 hours. An improvement, considered to be at least 10-15dB
in two adjacent frequencies, can occur in the early stages Ménière's
disease, usually in the lower frequencies, but in long term Ménière's
less effect is seen.
The glycerol acts as a diuretic and shows a purely osmotic action in
the reduction of the intra-labyrinthine pressure demonstrating that
endolymphatic hydrops contributes to the hearing loss associated with
Ménière's diease on a mechanical basis.
No glycerol effect is seen in normal subjects or in other types of
cochlear dysfunction. A positive glycerol test indicates a
reversibility and that a regime of diuretic medication may be of
some benefit.
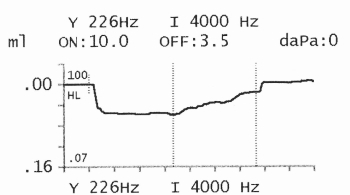
Acoustic
Reflex Threshold (ART)
 The acoustic reflex is the involuntary
contractions of the stapedius and the tensor tympani muscles (the
middle ear ossicular chain muscles) to high intensity sounds. This
reflex is used to reduce the amount of sound energy reaching the organ
of hearing, the cochlea. The reflex is seen bilaterally (in both ears)
irrespective of which ear is presented with the loud stimulus. The acoustic reflex is the involuntary
contractions of the stapedius and the tensor tympani muscles (the
middle ear ossicular chain muscles) to high intensity sounds. This
reflex is used to reduce the amount of sound energy reaching the organ
of hearing, the cochlea. The reflex is seen bilaterally (in both ears)
irrespective of which ear is presented with the loud stimulus.
A probe from a tympanometer is placed in the ear canal and the pressure
is equalised with the middle ear pressure. Brief loud tones (or mixed
frequency stimulus like 'white noise') can be presented to the ear with
the probe (ipsilateral) or the opposite side to the probe
(contralateral), if the sound is loud enough to evoke an involuntary
response the ear drum will be moved inwards and detected by the
tympanometer.
By obtaining the ART for various frequencies, both ipsi and
contralaterally, the site of lesion may be suggested, however further
testing with other methods are required for confirmation.
Acoustic
Reflex Decay
  Similar to ART a sound
stimulus is presented to the ear at 10dB above the ART so that a
definite reflex is be seen. The stimulus is presented continuously for
10 seconds and the reflex amplitude is measured. In a normal subject
there should be no or very little amplitude loss (decay) and so 500Hz
or 1KHz is used as some decay may occur in higher frequencies. Similar to ART a sound
stimulus is presented to the ear at 10dB above the ART so that a
definite reflex is be seen. The stimulus is presented continuously for
10 seconds and the reflex amplitude is measured. In a normal subject
there should be no or very little amplitude loss (decay) and so 500Hz
or 1KHz is used as some decay may occur in higher frequencies.
If the amplitude of the reflex decays more than 50% within 5 seconds it
is considered an abnormal result. This abnormal decay would then lead
us to suspect a retrocochlear lesion.
|
|